Almonds and Spinach as a Path to Atherosclerosis and High Cholesterol?
Amaranth, spinach, sweet potatoes, radishes, beet, almonds and other so-called superfoods can be a surefire route to health damage, chronic inflammation, high cholesterol, atherosclerosis, and heart attack. Don't you believe? Still think these are super healthy foods? Have you ever heard of oxalic acid or oxalates?
So let's look at it through the lens of recent studies. Let's start with a prospective study investigating the effect of dietary oxalate intake on atherosclerosis over a period of ten years, depending on calcium intake. Why did the authors choose this particular combination? Because oxalate occurs either as oxalic acid or bound to some mineral element, most commonly calcium. Calcium oxalate is the material that forms kidney stones as well as gallstones. Here, however, the binding to calcium is used even before processing in the digestive tract. If oxalate is already bound in the intestines, its absorption and flooding of the liver with oxalate from food will be limited. But food is not the only source of oxalates. The body itself produces oxalates and gets rid of them with the help of the kidneys. As you will see below, it is not good to overload this system, so it seems advisable to limit foods containing large amounts of oxalates.
If you argue that atherosclerosis is caused by cholesterol after all, then read my older post on cholesterol first. Cholesterol doesn't really play a major role here. Oxalates seem to play a much more significant role, the result of the study is unequivocal. If the intake of oxalates in the diet is higher than 220 mg per day, then the risk of cardiovascular disease is increased by 47%. But that's not all, with insufficient calcium intake (below 1000 mg/day), the risk increases to more than double (2.42 times). With a lack of calcium, even a daily intake of oxalate of about 150 mg is dangerous and increases the probability of a heart attack by twice as much compared to the group with the lowest intake of oxalates and sufficient calcium content in the diet.
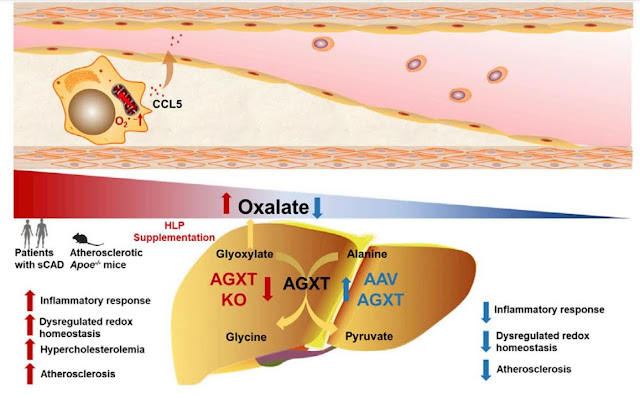 |
| Graphic abstract describing the effect of oxalates on atherosclerosis. |
Why? What mechanism causes this? The study entitled "Disregulated oxalate metabolism is a driver and therapeutic target in atherosclerosis" can answer that. The authors of the study investigated the influence of enzymes related to the breakdown of oxalate in the liver and found interesting connections. The main enzyme responsible for the processing of oxalates is the AGXT enzyme, and they created a mouse model in which they genetically suppressed this enzyme in a targeted manner and thus increased the oxalate load in a targeted manner. They compared this with an increased intake of oxalates or their precursors in the diet. Genetic suppression of the AGXT enzyme did increase atherosclerosis, but only in males. Females did not respond to this intervention. This is very interesting and the internal production of oxalates alone is not a sufficient stimulus. They also compared a standard mouse diet versus a so-called Western diet similar to the modern human diet. There it became clear that the modern human diet promotes atherosclerosis. Substances from which the body produces oxalate itself (here hydroxyproline) also support the development of atherosclerosis.
 |
| Glycine to oxalate ratio in mice on standard diet (SD) and western human diet (WD), you see a decrease in glycine and an increase in oxalate. |
 |
| Glycine to oxalate ratio in patients with coronary artery disease (sCAD). |
The AGXT enzyme processes glyoxylate (a precursor of oxalate) into the amino acid glycine and thus reduces the conversion of glyoxylate to oxalate by its activity. We already know that glycine decreases with increasing age, perhaps because the activity of the AGXT enzyme decreases with age, and this increases the likelihood of cardiovascular diseases for us, men in particular. However, the ratio of glycine to oxalate decreases even with increased oxalate consumption. The main finding of the study is that oxalate causes damage to the activity of mitochondria and peroxisomes, this is manifested by increased superoxide production, damage to the inner wall of blood vessels, inflammation and increased cholesterol production. Genetic activation of the AGXT enzyme will reduce the burden of oxalates and reduce oxidative stress and inflammation, thus reducing the risk of atherosclerosis.
 |
| Genetic activation of AGXT counteracts atherosclerosis and reduces superoxide production in the inner wall of blood vessels. |
Did I convince you? Oxalates are definitely not friendly. It is better to avoid them, definitely not eat them and think that all natural products are healthy. And which foods contain the most oxalates? Look for yourself in the tables available on the Internet.
References:
Dietary oxalate to calcium ratio and incident cardiovascular events
Dysregulated oxalate metabolism is a driver and therapeutic target in atherosclerosis



Comments
Post a Comment