Sugar prolongs the life of cells in the digestive tract, but it's probably not good !
Whenever I add hypoxia to a search engine request for some metabolic connections, the search engine always comes up with something interesting. As an example, this is the result of a search for a link between oxygen deficiency and sugar and fructose metabolism.
Sugar or sucrose, a disaccharide composed of glucose and fructose, has interesting effects on the lifespan of cells lining the digestive system. I have discussed fructose and its effects here and here. Today, we'll look at an interesting study in mice that shows how fructose affects cell survival in relative oxygen deprivation, i.e. hypoxia. But presumably this is also true elsewhere in the body during pseudo-hypoxia caused by, for example, the auto-oxidation aldehyde products of polyunsaturated fats, i.e. MDA, 4-HNE or 9-ONA. We'll see that fructose is definitely involved as well.
This also applies to high-fructose corn syrup (HFCS). This should have essentially the same properties as sugar, but there is information that it is more harmful than sugar. Undeclared residues of reactants from production may be to blame, after all it is not a natural product. Glucose is also a sugar, but its effects on metabolism do not seem to be as problematic. The main actor here is fructose.
 |
| This is what the surface of the small intestine looks like with the protrusions (villi). |
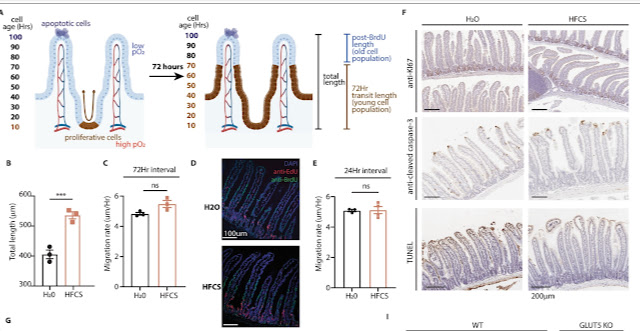
What does the surface of the small intestine actually look like? It is full of protrusions that not only significantly increase the surface area for nutrient absorption, but also ensure the constant renewal of cells on the surface. New cells originate at the foot of the protuberances and gradually travel towards the tip of the protuberance. At the end, they die and fall off. From birth to death it takes about 100 hours, or 4 days. Every 4 days, the cells on the surface of the intestinal wall completely renew themselves. Fructose in the diet causes the protuberances to elongate, but the rate at which the cells on the protuberance move remains the same. Thus, the life span of the cells is extended. How is this possible?
As the blood supply, and therefore the oxygen supply, deteriorates towards the end of the protrusion, the cells gradually lose access to oxygen as they travel and are exposed to hypoxia. They last a while and then die. It's a normal process. However, fructose will affect this by reprogramming the cell's metabolism to anaerobic, i.e. one that doesn't need any oxygen. This will cause the cells to survive in the absence of oxygen and the protuberances will lengthen. The surface area of the intestine will increase, more nutrients will be absorbed in the upper parts of the small intestine and less will reach the lower intestine (where the anti-obesity hormone GLP-1 is also produced), the colon and the stool. Moreover, as we already know, this anaerobic metabolism is based on the production of lactate and fat, both of which are produced from glucose. Interestingly, fructose is hardly metabolized. It enters the cell via the GLUT5 transporter and is converted to F1P. This causes suppression of the function of one important enzyme, pyruvate kinase (PKM2). But it only shows up in mild hypoxia. If there's enough oxygen, nothing special happens. It is only when oxygen deprivation creates the conditions for fructose to suppress PKM2 through excess F1P and thereby over-activate the transcription factor HIF-1, a change in the expression of many genes related to survival in oxygen deprivation. This is likely related to reduced H2O2 production when PKM2 activity is suppressed.
 |
| Fructose increases viability and reduces cell death (cytotoxicity) in the absence of oxygen (from 21% O2 to 4% O2 or chemical activation of apoptosis/death-stau). |
How fructose changes metabolism during hypoxia can be seen in this heat map, which shows the changes in the levels of many metabolic intermediates in different situations, normoxia, hypoxia and all without and with fructose (Fru):
 |
| Normoxia on the left, hypoxia on the right. The combination of hypoxia and fructose has a tremendous effect on cell metabolism (right quarter, the Glc+Fru graph). |
By a more detailed analysis of this map we can clearly see how fructose under hypoxia will increase the production of lactate (according to radioactive tracing from glucose, not from fructose) and fatty acids (palmitic acid, stearic acid, oleic acid). It also stops or reverses the running of succinate dehydrogenase SDH (which triggers gene reprogramming by HIF-1), this can be seen by comparing the levels of succinate and fumarate (a product of SDH), also how glucose, fructose and sorbitol (an intermediate of the polyol pathway) levels increase.
 |
| What fat + sugar (HFHC) versus water do to the small intestine. |
What to add, sugar increases the energy use of food, increases fat production from glucose, promotes cell survival without oxygen, reduces the production of hydrogen peroxide and promotes obesity. It's good for hibernating animals, it can also be useful for mitigating heart damage during heart attacks or hiking in the high mountains, but it's not so good for obesity. Fructose alters the length of the gut wall protrusions, changes the area that is in contact with nutrients and alters the metabolism of gut cells. It increases cell lifespan and cell viability, thereby also promoting the formation and growth of tumours in the gut. In the body, fructose can then promote the tendency of cells to metabolise without using oxygen, pseudohypoxia. Interestingly, bee honey, which is high in fructose, probably also contains substances that compensate for its negative effects. The bees just know what to do and how to do it. Perhaps they suspects that it is not good to combine fructose with polyunsaturated oils, which spontaneously oxidize to aldehydes. This combination seems to be a major source of chronic health problems.
Addendum:
The influence of fructose on the quality of the intestinal wall could also be medicinal. You really don't want a leaky or inflamed gut wall. Some researchers seem to be looking for, and successfully finding, drugs that activate HIF-1 in the intestinal epithelium, which is exactly what fructose does. Other researchers are investigating whether plant flavonols would work on a leaky and inflamed gut. But they have the exact opposite effect, blocking the expression of HIF-1 and thus can be dangerous. I wonder, didn't nature come up with this by combining flavonols with fructose, because each of these substances, administered alone, can be harmful?
References:
Dietary fructose improves intestinal cell survival and nutrient absorption
Pyruvate kinase M2 is a PHD3-stimulated coactivator for hypoxia-inducible factor 1



Comments
Post a Comment