Insulin resistance is caused by a lack of hydrogen peroxide in the cell !
Hydrogen peroxide H2O2 increases phosphorylation (activation) and slows down dephosphorylation (deactivation) of the insulin receptor, thereby increases its sensitivity to insulin and reduces insulin resistance. Don't you believe it? But not only that, it also keeps the suppression of insulin receptor sensitivity working after it has encountered high insulin levels, so it may also maintain insulin resistance. Let's take a closer look at this. We can't do it without the details from the scientific studies, but no worries. I'll try to make this idea of mine, which I think is heretical for now, understandable. In fact, I wrote a very similar explanation two years ago, only it lacked the adaptive mechanism of insulin receptors, which was unknown at the time.
 |
| Schematic of a negative feedback insulin receptor that functions as a signal compressor. |
 |
| Signal compressor function, if a long Release Time is set, then the sensitivity (Gain) is reduced for a long time after any signal peak. |
So we must first clarify how signal compression works. Signal compressors are mostly used in sound processing in studios and on stage. As a casual sound engineer, I have some experience with this; it's not easy to set up a compressor properly to smooth out sound and make it pleasant, so that the listener doesn't actually know the sound is going through compression at all. Normally the compressor densifies the sound, making the music or speech seem louder, but a poorly set compressor can make the signal sound quieter, can cause instability in the sound level and therefore make the situation very bad. If a very long relaxation time is set, a short loud drum beat can cause the signal to be suppressed for a long time. And this can also happen with the insulin receptor.
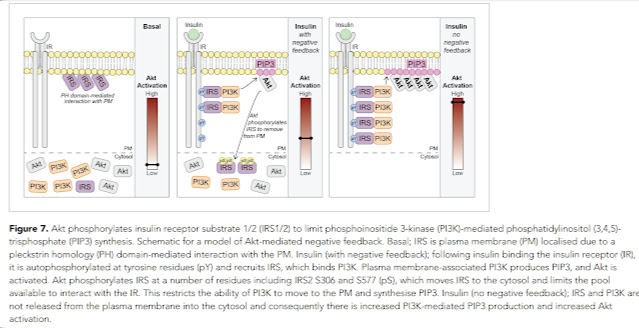
The insulin receptor is located in the cell membrane and works in such a way that the attached insulin molecule activates the AKT molecule on the other side of the membrane by controlled phosphorylation via IRS and PI3K molecules. The latter activates AKT, which then triggers all the necessary processes. But in addition, it also activates the labelling and movement of IRS molecules away from the cell membrane into the cytosol so that they are less available. This reduces the sensitivity of the receptor to insulin, which is a response to strong insulin stimulation. If the insulin signal wears off, the original sensitivity is restored after some time. But that's only if there's no intruder interfering with the parameter settings! For example, hydrogen peroxide, which increases the phosphorylation of the receptor and slows its relaxation, i.e. the return to the original sensitivity. But it's not actually an intruder, because if it's missing completely, it's also bad. There has to be just enough of it, I mentioned this once before in the context of controlling cellular metabolism.
 |
| Hydrogen peroxide prevents dephosphorylation (deactivation) of insulin-activated sites. |
 |
| Hydrogen peroxide enhances phosphorylation (activation) of insulin-activated sites. |
What happens if there is not enough hydrogen peroxide? The receptor won't react at all, it'll still be relaxed. The rate of receptor dephosphorylation and relaxation is so high without peroxide that it will cause only a very small and brief response to insulin. This is virtually a state of insulin resistance. This is reported in a study in mice. Genetically engineered mice with increased glutathione peroxidase activity have insulin resistance. Why? They have a hydrogen peroxide deficiency in their cells.
 |
| Comparison of mice with genetically increased GPX1 glutathione peroxidase activity (OE) with untreated (WT) mice. Effects on blood sugar, total weight, and adipose tissue weight were examined. |
 |
| Comparison of mice with genetically increased GPX1 glutathione peroxidase activity (OE) with untreated (WT) mice. Effect on hepatic insulin receptor sensitivity investigated. |
This condition probably also occurs in pseudohypoxia, when oxidative processes are replaced by fermentation and there is no production of superoxide O2-. When this occurs, many genes are switched on that increase fat and protein synthesis and are not controlled by insulin, overall causing obesity and other problems. Another common way to achieve pathologically low H2O2 levels is to activate glutathione peroxidase with fats. It's like the mice mentioned above, only it's not done genetically, but by diet. It can be done, for example, by excess of free fatty acids in the blood that are released in the morning from your fat stores, especially by excess of linoleic acid. This is even more pronounced when fasting or on a ketogenic diet, when a lot of fat is released into the blood, especially in obese people. This is because free fatty acids have a great ability to activate glutathione peroxidase and thus break down hydrogen peroxide rapidly. This is a normal defence because more superoxide is always produced when burning fat than when burning glucose. But the problem is that we have many times more omega-6 linoleic acid in our stored fat than our ancestors used to have. This manifests itself as seen in the muscle cell analysis of obese people with insulin resistance. There is "sand" in our enzyme gearbox in the form of aldehydes as products of secondary autooxidation of polyunsaturated fats. These interfere with the activity of the second mitochondrial complex (e.g. malonate created from MDA possibly blocks succinate debydrogenase SDH) and thus impede fat burning, reducing the amount of superoxide and hydrogen peroxide produced. In addition, they also increase the level of free fatty acids, so they increase the activity of glutathione peroxidase and further reduce the level of hydrogen peroxide, which, as we already know, accelerates relaxation of insulin receptors and reduces their sensitivity.
And in this state we have a breakfast full of fast carbohydrates in the morning. Insulin spikes, but with little receptor sensitivity, it causes glucose levels to rise, so it gets into the unprepared cell and starts producing large amounts of superoxide and hydrogen peroxide. This causes both further auto-oxidation of linoleic acid to aldehydes ("sand") but mainly causes an increase in sensitivity and slowing of insulin receptor responses. The latter are at this moment set to a strong signal and try to dampen it as much as possible, This situation will be fixed for a longer time and the receptors will remain suppressed. After a period of time after the meal, the receptors relax, but they return to the other extreme, the low sensitivity caused by the lack of hydrogen peroxide. Thus, there are two states of insulin resistance, one is induced by peroxide deficiency during fasting (or keto dieting) and the other is induced by peroxide excess during eating. There may be a brief moment in between these states when peroxide levels are normal and receptors may be functioning properly, but it is completely insignificant. Proper functioning of insulin receptors requires the right amount of hydrogen peroxide, i.e. neither too little nor too much.
This cycling is ongoing, from one state of insulin resistance to another. We already know how to get out of this cycle. It's oxidative therapies. Particularly before meals, when they increase the sensitivity of insulin receptors at a time when they are controlled by peroxide deficiency caused by excessive glutathione peroxidase activity. I've discussed this many times here, there are therapies with highly diluted hydrogen peroxide or ozone therapies. Now we know they make sense. And we have a mechanistic explanation for how they directly affect such a strange cellular behaviors as insulin resistance. MCT oil supplementation, especially during the morning before a major meal, has the same effect on increasing insulin receptor sensitivity. The direct effect of reducing insulin resistance is measurable and anyone can test this by following this procedure.
Addendum:
Fructose (sugar) blocks the activity of the PKM2 enzyme and thus reduces the formation of hydrogen peroxide on PDHC in the absence of oxygen and blocks the supply of pyruvate to mitochondria. This activates HIF-1, the cell's metabolism changes, and the cell is more likely to survive hypoxia. This will also increase the risk of cancer and it means that the lack of H2O2 is a really big problem. See the following post.
References:
Hydrogen Peroxide Flips the Switch - Fire In A Bottle
Development of insulin resistance and obesity in mice overexpressing cellular glutathione peroxidase
Akt phosphorylates insulin receptor substrate to limit PI3K-mediated PIP3 synthesis




Comments
Post a Comment